Welcome, fellow dentists! As the field of implant dentistry continues to evolve, so must our understanding of the technology behind it. Dental implants are the foundation of modern restorative dentistry, providing patients with a durable and aesthetically pleasing solution to tooth loss. But beyond the beautiful restoration lies a sophisticated system of interconnected parts.
This detailed guide will break down the dental implant system into its basic components. We will explore the function, design variations, and clinical significance of each part. We will delve into the implant body (screw), abutment, and final restoration, providing you with a clear, structured framework to enhance your practice.
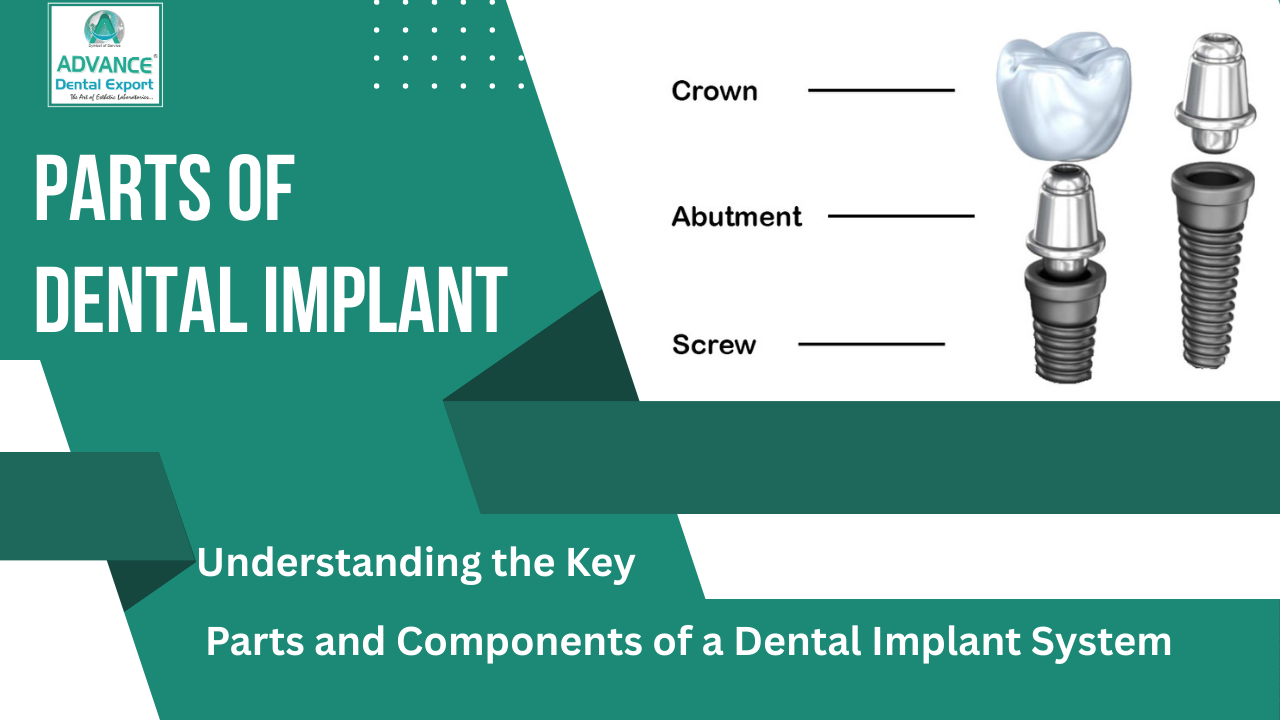
Three Core Components of a Dental Implant System
Think of a dental implant system as a three-part machine designed to mimic the structure of a natural tooth. Each part has a different role, but they must work together to achieve a successful outcome. There are three main components:
- Implant Body (or Fixture): This is the foundation, the original replacement that integrates with the jawbone.
- Abutment: This acts as a connector, bridging the implant body to the final restoration.
- Prosthetic Restoration: This is the visible, functional part, crown, bridge, or denture that replaces the missing tooth or teeth.
Let’s dive into each of these components in detail.
Implant Body: The Foundation of a New Tooth
The implant body is the main part of the system. It is a titanium or titanium-alloy screw-shaped fixture that is surgically placed into the jawbone. Its primary function is to serve as an anchor for the remaining components and integrate with the surrounding bone through a process called osseointegration.
Understanding Osseointegration
Osseointegration is a biological process in which living bone tissue fuses directly with the surface of the implant body. This creates a stable and rigid anchor, similar to the root of a natural tooth. The success of the implant depends entirely on this process. This is a phenomenon that was first described by Professor Per-Ingvar Bränmark in the mid-20th century, which revolutionized the field of dentistry.
Key Characteristics of the Implant Body
When you select an implant body, you consider several crucial factors:
Material
Titanium: Pure titanium and titanium alloys (such as Ti-6Al-4V) are the gold standard. They are biocompatible, strong, and highly resistant to corrosion. They promote excellent osseointegration.
Zirconia : Zirconia implants are a ceramic alternative. They offer a metal-free option and a white color that can be beneficial in aesthetically demanding areas with thin gingival tissue. However, they are less commonly used and have a different biomechanical profile.
Surface Treatment
The surface of the implant is not smooth. Manufacturers use a variety of treatments to enhance osseointegration. These include:
- Sandblasting and acid-etching (SLA): This process creates a micro-roughened surface, which increases the surface area for bone cells to attach to.
- Plasma Spraying: This technique applies a thin layer of porous titanium to the surface, further increasing its roughness and bio-interactivity.
- Anodization: This electrochemical process creates a thick, porous oxide layer on the titanium surface.
Implant Shape and Thread Design
Tapered vs. straight-walled Implant : Tapered implants are narrow at the apical end and wide at the coronal end. This shape often mimics the shape of a natural tooth root, allowing for easy placement in narrow spaces. Straight-walled implants, on the other hand, provide excellent stability and are often used in dense bone.
Thread design: The threads on the implant body help secure it to the bone during placement and increase the surface area for osseointegration. Various thread designs exist, ranging from fine to coarse, each with specific biomechanical advantages for different bone densities.
Dimensions (Length and Diameter)
Choosing the right implant length and diameter is important.
Length: A longer implant provides more surface area for osseointegration but also requires sufficient bone height.
Diameter: A wider implant provides more stability and may be a better option for molars that experience high occlusal forces.
Explore Our Restorations
Connection Type
This is how the implant body connects to the abutment. There are several popular types of connections:
External Hex: A hexagonal post on top of the implant body. It was one of the early designs, but it is now less common due to the potential for screw loosening and micromotion.
Internal Hex: A hexagonal recess inside the implant body. This design provides a more stable, anti-rotational connection and is widely used today.
Internal Morse Taper: This friction-fit connection creates a very strong, tight seal between the implant and the abutment. It reduces micromotion and bacterial leakage, which is important for long-term health. Many modern systems use variations of this design.
Tri-Channel/Octa-Channel: These are proprietary systems with three or eight channels, respectively, for anti-rotational protection.
Abutment: The Critical Link
Another key component of a dental implant system is the abutment. It is a connector that screws or cements onto the implant body, protruding from the gum line. Its primary function is to support the final prosthetic restoration. The choice of abutment is often determined by the specific clinical situation, including the location of the implant, the depth of the gum tissue, and the type of restoration.
Types of Abutments
You have a wide range of abutment options to choose from, each with a specific purpose:
- Standard (stock) abutments: These are pre-manufactured abutments that are available in a variety of sizes, shapes, and angulations. They are a cost-effective option for straight cases, especially in areas with good tissue depth and alignment.
- Custom abutments: These abutments are digitally designed or milled to the specific patient anatomy. The dental lab creates them based on a digital scan or impression. Custom abutments offer significant advantages such as:
- Improved aesthetics: You can control the emergence profile to create a natural-looking contour where the crown meets the gum tissue. This is especially important for front teeth.
- Enhanced function: You can adjust the abutment to align perfectly with the opposing occlusion, reducing stress on the restoration and implant.
- Excellent hygiene: The customized shape of the abutment and crown margin makes cleaning easier for the patient.
- Healing abutments: After the implant body is placed, you often use a healing abutment. This is a temporary component that screws into the implant. Its purpose is to shape the gingival tissue and create an ideal emergence profile for the final restoration. You usually remove it when you are ready to place the final abutment and crown.
- Temporary abutments: You use these to support the temporary crown during the healing phase. This allows the patient to have a functional and aesthetic tooth while the implant integrates with the bone. These can be made of plastic or titanium.
Abutment Material
- Titanium: Like implant bodies, titanium is a popular choice for abutments. It is strong, biocompatible, and durable.
- Zirconia: Zirconia abutments are often used in aesthetic areas. Their tooth-like color prevents greyish shadows from showing through the gum tissue, which is an important concern, especially in patients with thin biotypes. You often use them to create monolithic, metal-free restorations with zirconia crowns.
- Gold-colored titanium nitride (TiN): Some abutments have a gold-colored coating. This also helps to mask the gray color of the titanium, which provides a better aesthetic result in certain situations.
Prosthetic Restoration: The Crown, Bridge, or Denture
The final component of a dental implant system is the prosthetic restoration. This is what the patient sees and uses to chew. The type of restoration depends on the number of missing teeth and the patient's specific needs.
Types of Restorations Supported by Implants
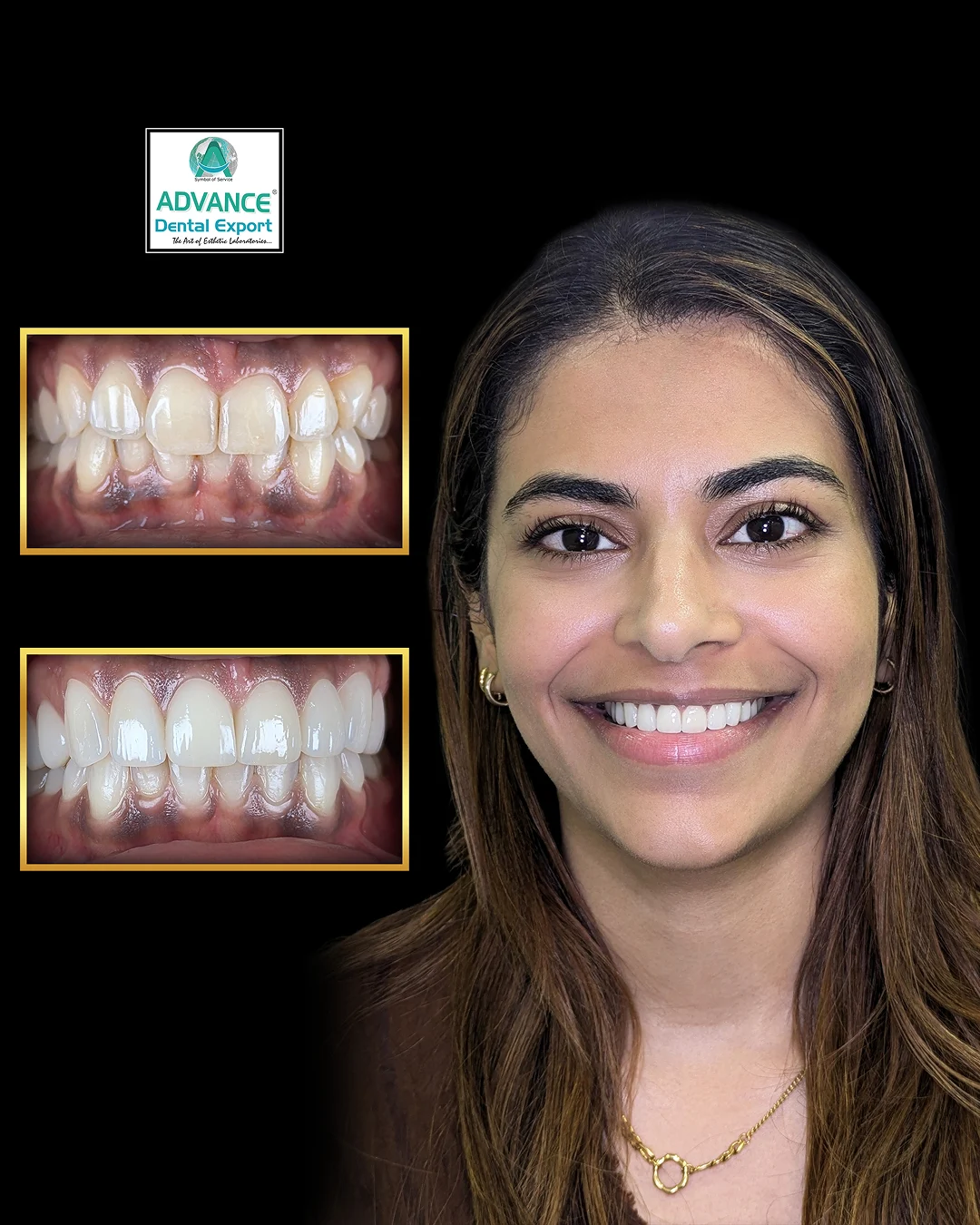
- Single Crowns: This is the most common restoration method for a single missing tooth. The crown is either cemented or screwed onto an abutment.
- Cement-Retained Crowns: The crown is cemented onto an abutment, much like you would cement a crown onto a natural tooth. This method offers excellent aesthetics because there is no visible screw hole. However, it requires careful cement removal to prevent peri-implantitis.
- Screw-Retained Crowns: The crown and abutment are often a single unit, screwed directly into the implant body. The screw access hole is then filled with a restorative material such as composite. This provides easy retrieval for maintenance or repair.
- Implant-supported bridges: For many nearby missing teeth, you can use an implant-supported bridge. Two or more implants support a fixed dental bridge, eliminating the need to prepare nearby natural teeth. This is a significant advantage over traditional bridges. Implant-supported dentures: For dentulous patients, implants can provide incredible stability for dentures.
- Overdentures: Two to four implants are placed, and denture clips are attached to the attachments on top of the implants. This provides a removable but highly stable option, which improves chewing ability and confidence.
- Fixed Full Arch Bridge (All-on-4 or All-on-6): This technique uses four or six implants to support a fixed, non-removable full arch prosthesis. This provides the closest feel to having natural teeth.
Materials for the Prosthetic Restoration
- Porcelain-fused-to-metal (PFM) : This traditional option provides a strong metal framework with a porcelain layer for aesthetics. It is durable but can sometimes show a gray line at the gum line.
- All-ceramic (zirconia, Emax): This material has become the standard for modern restorations. Zirconia is exceptionally strong and is ideal for posterior crowns and bridges. Lithium disilicate (Emax) offers superior translucency and is often the material of choice for highly aesthetic anterior crowns.
Looking for a trusted lab partner? Get high-precision restorations from Advance Dental Export
Role of the Dental Laboratory in Implant Dentistry
As a dentist, your partnership with a skilled dental laboratory is critical to successful outcomes. Lab technicians specialize in creating final prosthetic restorations and often custom abutments. You provide them with an accurate impression or digital scan, and they use their expertise to create a restoration that fits perfectly, functions, and looks natural.
Here’s what you need to communicate with your lab partner for the best results:
- Accurate impression or digital scan: The foundation of a good restoration is an accurate representation of the intraoral situation.
- Abutment type: Specify whether you need a stock, custom, or temporary abutment.
- Material selection: Discuss the advantages and disadvantages of different materials (zirconia, Amex, PFM) with your lab to select the best option for the case.
- Shade and aesthetic details: Provide clear photos and shade tabs to ensure the final restoration matches the patient’s existing teeth.
Screws and Components That Connect Everything
We have covered three main parts, but a full understanding requires acknowledging the smaller yet equally important components:
- Cover screw: A small screw placed into the implant body after surgery, used to seal it and prevent tissue from growing into the internal connection during the healing phase.
- Healing collar: A type of healing abutment, it is a small, cylindrical component that protrudes from the gum tissue to guide the healing of the soft tissue around the implant site.
- Abutment screw: The screw that attaches the abutment to the implant body. The torque setting for this screw is important to prevent loosening and ensure a stable connection.
- Prosthetic screw: A screw that holds a screw-retained crown or bridge to the implant.
Conclusion
Mastering the intricacies of the dental implant system is a journey of continuous learning. From the micro-rough surface of a titanium implant body to the finely crafted emergence profile of a custom zirconia abutment, every detail contributes to the long-term success of a restoration. We’ve explored the three main components – the implant body, the abutment, and the prosthetic restoration – along with the important roles they play and the variations you can choose from.
By understanding the biomechanics and materials behind each part, you can confidently plan and implement a treatment that not only restores function and aesthetics but also stands the test of time. A well-informed dentist is the best advocate for their patients, and a strong partnership with a skilled dental lab completes the circle of care.We hope this comprehensive guide will serve as a valuable resource for your practice.
FAQs
What is a dental implant?
A dental implant is a small, screw-shaped post, typically made of titanium, that is surgically placed into the jawbone. It serves as a strong, stable root for a replacement tooth or teeth.
What are the key components of a dental implant system?
A dental implant system has three main parts: Implant (Fixture), Abutment & Crown (Prosthesis).
Which material is best for dental implants?
Zirconia is the best dental implant material for patients who have metal allergies or prefer a non-metallic look. It is highly biocompatible, meaning the body accepts it well. Titanium is another good option, widely used and a successful material for dental implants.
What types of dental restorations are supported by implants?
Dental implants can support a variety of restorations, including: Single Crowns, Implant-Supported Bridges, Full Arch (All-on-4 or All-on-6), and Implant-Supported Dentures.